(407) 752-0436 (Grandpa Mike)
Frequent medicare questions answered!

Is my Medicare Advantage Plan (MAPD) the same as a Medicare Supplement plan?
No. A Medicare Advantage plan is different than a Medicare Supplement plan in that in most cases, a Medicare Advantage Plan may have a $0 premium without a monthly cost (aside from co-pays for specialists, hospitals, etc), whereas Supplement plans usually have monthly premiums along with a separate part D monthly premium for drug coverage. (FYI, both plans have co-pays for prescription drugs). In simple terms, a Medicare Supplement plan is more of a “pre-pay” plan which means you pay your same monthly premium (usually between $100 to $250 a month and then add on your Part D premiums around an estimated $50 a month, no matter how many visits you make to your Primary Care Doctor. A Medicare Advantage plan (MAPD) is more of a “pay as you go” plan and when doing a side-by-side comparison, for most clients, a MAPD plan has a lower monthly cost, whereas for some, a Supplement plan may be better. During any appointment we will discuss these costs differences and always allow our clients to make their own best-informed decision. It is important to know that Medicare Supplement insurance, also known as Medigap or MedSup, is sold through private insurance companies, and is not comprehensive medical coverage. Instead, Medigap functions as supplemental coverage to Original Medicare. Current Medigap plans don't include prescription drug coverage. We will help you compare both options together to allow for you to make the best-informed decision for you and your family. Call us at (407) 752-0436 or contact us below.

Can I change my Medicare Advantage plan and when are the Enrollment periods?
If you want to switch between one Medicare Advantage plan to another, you can do so each year during the Annual Election Period (AEP) or the Open Enrollment Period (OEP), which runs October 15 to December 7 and the annual Medicare Advantage Open Enrollment Period (OEP), which runs January 1 – March 31 every year. If you are new to Medicare, you can switch MA plans during an individualized Medicare Advantage Open Enrollment Period that runs during the first 3 months you enroll in Medicare. You may also be able to switch plans during a Special Enrollment Period based on your plans star rating if it has a 5 star rating. Once you select a new plan to enroll in, you’ll be disenrolled automatically from your old plan when your new plan’s coverage begins. You do not have to contact your old plan to disenroll unless it is a Medicare Supplement plan of which cannot overlap with a Medicare Advantage plan.
The Medicare Advantage Open Enrollment Period provides additional opportunities to change your Medicare Advantage plan outside the Annual Election Period Oct 15 – Dec 7. The annual Medicare Advantage Open Enrollment Period (OEP) allows anyone enrolled in a Medicare Advantage plan on January 1 the opportunity to change plans. The annual OEP runs from Jan 1- Mar 31. There is also an individualized Medicare Advantage open enrollment period (IEP) that’s limited to new Medicare beneficiaries with both Medicare Parts A & B who enroll in a MA plan during their initial coverage election period. Call (407) 752-0436 or contact us.
Which Medicare card do I show my Doctor?
Be careful that you do not give your Provider the Wrong Medicare ID Card! This one has several versions of easy Medicare mistakes. If you have chosen Medicare as your primary coverage then you will present your Original Medicare card (and Medigap card) to your provider at the time of service. If you enrolled in a Medicare Advantage plan (Part C) though, that plan pays INSTEAD OF Medicare. People don’t realize this and they give their doctor their Medicare card by mistake. What does Medicare do? In most cases they will deny all of the claims because those bills should have gone to your new Medicare Advantage Company. We have also had cases where a Medicare beneficiary is rushed to the hospital. His or her spouse digs through their wallet and pulls out the “old original Medicare card” for the hospital. The hospital sends all the bills to Medicare because they assume the spouse is presenting the correct coverage. It’s particularly awful because treatment in the hospital can be billed from a variety of places – radiology, anesthesiology, physical therapy, the hospital itself. Each of those bills then have to be corrected separately which can take you several hours by phone to straighten out. We strongly suggest if you are enrolled in a new Medicare Advantage plan, put your red, white and blue original Medicare card away in a safe place, out of sight and out mind. You will not be using it unless you later decide to drop your new Medicare Advantage plan. Give your providers only your new Medicare Advantage card which will save you a lot of headaches. Call us anytime you need help at (407) 752-0436 for more answers to your questions or contact us below. We are here to serve you!

What does Part A/B/C/D/ mean to me?
We will explain this in simple terms without adding to the already confusing aspects on the different parts.
Part A: Part A is your hospital coverage and anything that involves an overnight stay or hospital visit. This would be considered an "inpatient" visit.
Part B: Part B is anything that involves a same day visit (non-hospital) such as a visit to your primary care Doctor, going to a specialist, lab work, x-rays, urgent care, etc. This is considered an "outpatient visit".
Part C: Part C is when you decide to get your Medicare benefits from a Medicare Advantage Plan, also called Part C. Remember, you still have Medicare parts A and B if you enroll in a Medicare Advantage Plan. This means that you must still pay your monthly Part B premium (and your Part A premium if you have one). Each Medicare Advantage Plan must provide all Part A and Part B services covered by Original Medicare, but they can do so with different rules, costs, and restrictions that can affect how and when you receive care.
Part D: Part D is your prescription drug coverage and all MAPD plans have drug coverage included in their plans, the "D" standing for "D" Drug coverage. Your drug co-pays are then determined by various "tiers" with tiers 1 and 2 having the lowest co-pays and in some cases with a $0 co-pay. Your Rx bin number will be on your new MAPD card. Call us at (407) 752-0436 if you have further questions or contact us.

How does Medicare work with Medicaid?
The State of Florida offers a variety of Medicaid programs, with eligibility and coverage specifics varying by state. If you qualify for a Medicaid program, it may help pay for costs and services that Medicare does not cover (including co-pays on your new MAPD or D-SNP "Dual Special Needs Plan" which you may qualify for). Here are a few examples of how Medicaid can work with Medicare.
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors’ visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last. When you visit a provider or facility that takes both forms of insurance, Medicare will pay first and Medicaid may cover your Medicare cost-sharing, including co-insurances and co-pays. Here are a few examples of how Medicaid can work with Medicare, also called in the industry as "Medi-Medi".
Medicaid can provide premium assistance: In many cases, if you have Medicare and Medicaid, you may automatically be enrolled in a Medicare Savings Program (MSP) or we may have to apply for you in some cases. MSPs pay your Medicare Part B premium, and may offer additional assistance. Medicaid can provide cost-sharing assistance: Depending on your income, you may qualify for the Qualified Medicare Beneficiary (QMB) MSP. If you are enrolled in QMB, you do not pay Medicare cost-sharing, which includes deductibles, co-insurances, and co-pays.
Medicaid can provide prescription drug assistance: Dual eligible individuals may be automatically enrolled in the Extra Help program (by the Social Security Administration) to help with your prescription drug costs or we may need to apply for you in some cases. This is called L.I.S. (low-income subsidy) and we can determine your eligibility level for you.
Feel free to call us at (407) 752-0436 to help determine your Medicaid eligibility level or contact us below.

Do I need a referral to see a specialist?
Yes and no! A written order from your primary care doctor (PCP) for you to see a specialist or get certain medical services is required in many Health Maintenance Organizations (HMOs), whereas a PPO most likely does not.
You need to get a referral before you can get medical care from anyone except your primary care doctor. If you don't get a referral first, the plan may not pay for the services. However, a Medicare Advantage Plan that is a PPO (Preferred Provider Organization), in most cases does not require a referral, but may have slightly higher costs on co-pays and co-insurance. In most cases, the cost difference may be well worth it in not needing your Primary Care Doctor to go through the referral process to see a specialist as an HMO plan requires. This decision is made by you as to what best fits your own unique needs. But even withing an HMO plan, most primary care Doctors have a group of specialists to refer you to based on your needs with a familiar "circle of specialists" that they direct your coordinated care with.
Remember, this is not referring to a Medicare Supplement Plan which in most cases a referral is not needed, but supplements do have monthly premiums that may or may not be cost productive for you. We are always here to help you with these calculations within a required SOA "Scope of Appointment" for each individual plan and can always answer any questions you may have.
For some clients who have a need to see various specialists, a PPO is preferred as to avoid the referral process and, in some cases, may open up a larger network of doctors even if a particular Doctor or Specialist is out of the plans network. When we are in appointment together, we will search your choice of Doctors and Specialists to make sure they are in network and provide you an easy transition if you are new to Medicare or with a transition into a new plan.
Please call us at (407) 752-0436 or contact us below and we will make Medicare easy for you at 65, or any age if qualified.

Are my drugs covered in my new plan?
As your personal agent we will go over every prescription drug that you take and check to make sure they are covered, along with the co-pays and various tiers. We will also explain the "Donut Hole" which is the phase of Part D coverage after the end of your initial coverage period. After falling into the donut hole, the amount you pay for your prescriptions increases. If you’ve noticed that you are suddenly paying more for your drugs, you may be in the donut hole. You enter the donut hole when your total drug costs—including what you and your plan have paid for your drugs—reach a certain limit. For most plans in 2019, this amount is $3,820. You generally pay more for your drugs during the coverage gap. However, as a result of health reform, there are federally funded discounts that help you pay for your drugs during the donut hole. In 2019, there is a 75% discount for most brand-name drugs, paid for by the manufacturer and the federal government. This means you pay the remaining 25% of the cost for brand-name drugs. Similarly, the government provides a 63% discount for generic drugs. This means you pay the remaining 37% of the cost for generics. (2020 will have slight adjustments).
Due to federal legislation, the donut hole is closed for brand-name drugs in 2019. This closure means that you will be responsible for 25% of the cost of your brand-name drugs in this coverage period. Although the donut hole for brand-name drugs has closed, you may still see a difference in cost between the initial coverage period and the donut hole. For example, if a drug’s total cost is $100 and you pay your plan’s $20 copay during the initial coverage period, you will be responsible for paying $25 (25% of $100) during the coverage gap. The donut hole will close for generic drugs in 2020, at which point you will be responsible for 25% of the cost of your generic drugs.
How do I get out of the donut hole?
In all Part D plans, after you have paid $5,100 in 2019 in out-of-pocket costs for covered drugs (this amount is just the amount you have paid, not the total drug costs that you and your plan have paid), you leave the donut hole and reach catastrophic coverage. During this period, you pay significantly lower copays or coinsurance for your covered drugs for the remainder of the year (most of our clients do not enter the hole). The out-of-pocket costs that help you reach catastrophic coverage include:
- Your deductible
- What you paid during the initial coverage period
- Almost the full cost of brand-name drugs (including the manufacturer’s discount) purchased during the coverage gap
- Amounts paid by others, including family members, most charities, and other persons on your behalf
- Amounts paid by State Pharmaceutical Assistance Programs (SPAPs), AIDS Drug Assistance Programs, and the Indian Health Service
Costs that do not help you reach catastrophic coverage include monthly premiums, the cost of non-covered drugs, the cost of covered drugs from pharmacies outside your plan’s network, and the 63% generic discount. During catastrophic coverage, you will pay 5% of the cost for each of your drugs, or $3.40 for generics and $8.50 for brand-name drugs (whichever is greater). Your Part D plan should keep track of how much money you have spent out of pocket for covered drugs and your progression through coverage periods—and this information should appear in your monthly statements. Note: If you have Extra Help, you do not have a coverage gap. You will pay different drug costs during the year. Your drug costs may also be different if you are enrolled in an SPAP. (slight adjustments for year 2020).

Who do I call when I have questions?
We highly recommend that whenever you have any questions regarding your Medicare plan that you contact us primarily and as a second choice you can always call the carriers number on the back of your new card.
The reason we recommend that you call us first is that we are very familiar with your own unique status and situation, whereas the carrier will have to be updated with all your details that we have already gone over with you and have in your file. This will save you a lot of time and energy. Secondly, we are appointed with all the available carriers in the State of Florida having a big bag of options and resources for you. Calling in your questions to one company alone is not necessarily the wrong call to make, but keep in mind that your conversation will be with a "captive" representative, meaning their options are tied to their company along, and cannot represent any other carrier or plan. This may limit your options as to what is best for you and your family. Call us at (407) 752-0436 with any questions!
What if it is after hours or I get your voice mail?
We are always available for your call and answer every call, every time. If we are on another call, with a client, and you get our voicemail, simply leave us a message and we will return your call the very same day. Your concerns are our concerns and we commit to you that we will always go the extra mile regardless of how many questions you may have. Please remember, it is our job to make sure you have more answers than you have questions and we enjoy helping you get answers to your questions, our passion is to help others.
Here is a list of quick yes and no answers to hold you off until we talk and go over your specific plan questions.
* Does my plan have a gym membership?
YES! Unless we told you in your enrollment that it does not.
* Do I need to re-enroll in my plan each year?
NO! Unless you are switching plans the carrier will automatically re-enroll you and any plans changes will be mailed to you with nothing on your part to do.
* Does my plan effect my Part B premium?
NO! Your new Medicare Advantage or Supplement plan has nothing to do with your Part B premium, this deduction was already determined by Social Security and any Part B cost increases are based upon your income and related to Social Security. Even thought your plan administers your Medicare, your Part B deduction would be the same with or without any Medicare Advantage or Supplemental plan (unless your plan has a premium other than $0). In most cases, especially with HMO plans, your 'premium' may be $0, whereas your Part B original Medicare premium was already established before joining any Advantage or Sup. plan.
* Why did my first prescription cost so much?
If your plan has a one-time RX deductible, this cost must be met first and then you will pay the co-pays according to the tier level that your drug is on. Keep in mind, most plans only have this once-a-year RX deductible for drugs that are in the Tier 3,4 and 5 category, and some plans have no deductible.
* What if my doctor moved, or is no longer in network?
Call us at (407) 752-0436 and we will help you find another primary care physician for that is part of our job duty.
* My Husband or Wife has passed & my income has changed.
It grieves us of such news as we hear this at times from Medicare clients. When you are ready, call us so that we can determine if your change of income qualifies you for any extra help. We have compassion and desire to help you through this difficult time, and if you qualify for extra help, it may be of some comfort for you in the time of trouble.
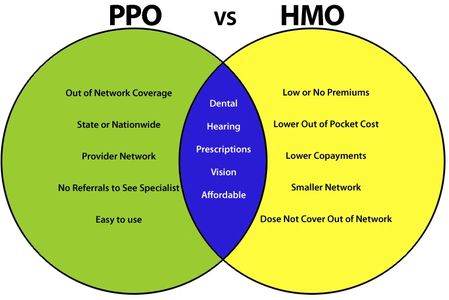
What's the difference in an HMO and PPO?
There are a lot of decisions to make when it comes to choosing a health insurance plan. One of the first decisions you will need to make is which type of plan is right for you.
You’ve probably heard the terms health maintenance organization (HMO) and preferred provider organization (PPO), but do you really understand the differences between the two? Which one is cheaper? Which one provides the coverage you need? To help you decide, we will lay out the basic features of HMOs and PPOs. Once you have a better understanding of each plan type and how it works, it will be much easier to choose the plan that’s best for you and your family. You can also call us at (407) 752-0436 for more help.
HMO plans typically have lower monthly premiums. You can also expect to pay less out-of-pocket. PPOs tend to have higher monthly premiums in exchange for the flexibility to use providers both in and out-of-network without a referral. Out-of-pocket medical costs can also run higher with a PPO .
An HMO gives you access to certain doctors and hospitals within its network. A network is made up of providers that have agreed to lower their rates for plan members and also meet quality standards. But unlike PPO plans, care under an HMO plan is covered only if you see a provider within that HMO’s network. There are few opportunities to see a non-network provider. There are also typically more restrictions for coverage than other plans, such as allowing only a certain number of visits, tests or treatments. Some other key points about HMO plans are as follows....
- Some plans may require you to select a primary care physician (PCP), who will determine what treatment you need.
- With some plans, you may need a PCP referral to be covered when you see a specialist or have a special test done.
- If you opt to see a doctor outside of an HMO network, there is no coverage, meaning you will have to pay the entire cost of medical services.
- Premiums are generally lower for HMO plans, and there is usually no deductible or a low one.
Some HMO plans don't require you to select a PCP or have a referral to see a specialist.
PPO plans provide more flexibility when picking a doctor or hospital. They also feature a network of providers, but there are fewer restrictions on seeing non-network providers. In addition, your PPO insurance will pay if you see a non-network provider, although it may be at a lower rate. Here are some key features within most PPO plans.....
- You can see the doctor or specialist you’d like without having to see a PCP first.
- You can see a doctor or go to a hospital outside the network and you may be covered. However, your benefits will be better if you stay in the PPO network.
- Premiums tend to be higher, and it’s common for there to be a deductible.
Plan Networks
A defining feature of HMO and PPO plans is that they both have networks. Networks are one way to lower health care costs – network providers agree to give discounts in exchange for access to a health plan’s members. This saves health insurers money, but it also saves health plan members money as well – savings for the insurer can translate to lower premiums, deductibles and co-pays. In general, PPO networks tend to be broader, including more doctors and hospitals than HMO plans, giving you more choice. However, networks will differ from insurer to insurer, and plan to plan, so it’s best to research each plan’s network before you decide. We will help you with that!
Primary Care Physicians
Most HMOs will require you to select a primary care physician, who will be the primary point of contact for your medical care. Your PCP will determine what treatments you need, and will refer you to specialists if he or she determines specialized care is medically necessary. Costs for specialists will not be covered without a PCP referral. In contrast, PPOs tend not to require selection of a PCP, and you can usually see a specialist without a referral, and still have these costs covered.
Coverage for Out-of-Network Care
For both PPO and HMO plans, your costs for care will be lowest if you receive it from in-network providers. The two types of plans differ considerably in coverage for services from providers outside the plan network. For HMOs, out-of-network services are usually not covered at all, except for emergencies. PPOs differ from HMOs in that PPO plans will usually provide some coverage for these types of services, but coverage for in-network providers will be much better.
Costs
The additional coverage and flexibility you get from a PPO means that PPO plans will generally cost more than HMO plans. When we think about health plan costs, we usually think about monthly premiums – HMO premiums will typically be lower than PPO premiums. Another cost to consider is a deductible. This is the amount of health care costs you must pay before your plan begins to cover your costs. Not all HMOs have deductibles, but when they do, they tend to be lower than PPO deductibles. Call us anytime at (407) 752-0436 if you need more help or contact us below.
What is the new OEP period?
The OEP allows beneficiaries who are enrolled in a Medicare Advantage Plan to make a one-time change. Beneficiaries can use the Medicare OEP to:
- Switch from one Medicare Advantage plan to another Medicare Advantage plan
- Disenroll from a Medicare Advantage plan and return to Original Medicare, with or without a Part D drug plan.
The Medicare OEP does not, however, allow a beneficiary to change from one Part D plan to another.
Medicare beneficiaries who enroll in Medicare Advantage plans sometimes find themselves stuck in a plan that they do not like. Although the plan’s Summary of Benefits covers the specifics of how the plan works, it’s all too easy for a beneficiary to misunderstand the rules or forget to check whether a certain doctor is in the network.
The Medicare OEP is a period at the beginning of each year when Medicare Advantage plan enrollees can make a one-time switch to a new plan.
Beginning in 2019, Medicare beneficiaries were able to use a period called the Medicare Advantage Open Enrollment Period (OEP) to make a one-time change.
This Medicare Advantage Open Enrollment Period is not new. It used to be a regular part of each Medicare year before the ACA legislation discontinued it. It allows individuals enrolled in a Medicare Advantage plan to make a one-time change early in the year.
The ACA law signed in 2010 ended the Medicare OEP and replaced it with a Medicare Advantage Dis-enrollment period that ran January 1st to February 14th. This period was different from the Medicare OEP in that it only allowed Medicare Advantage enrollees to go back to Original Medicare. It did not allow them to change from one Medicare Advantage plan to another.
That is now changing, and we are going back to the way it was before the ACA legislation. Let’s take a look at what changes you can make in 2019 when the OEP returns.
The reason for the change is that Medicare beneficiaries are often confused about Medicare Advantage plans. They don’t understand how these plans work or they may not realize the plan has a network. Some Medicare beneficiaries try to make their own plan changes without the help of a Medicare insurance expert. Therefore many do not know what they are getting into. They may overlook important factors without guidance or counsel from a Medicare professional.
They might unknowingly join a plan that one of their doctors doesn’t participate in. Some might also forget to check the plan’s drug formulary to make sure it covers all of their important medications. We can help you with this.
It’s also common for a beneficiary to not realize that Advantage plans require co-pays on the back end. They are so set on that plan’s low premium that they miss the rest of the facts about how the plan works. Then they have a hospital stay and get a bill for $1400 dollars and are shell-shocked. We discuss all these details beforehand.
Even beneficiaries who work closely with an agent who clearly explains that a plan is Medicare Advantage will still sometimes in their minds think of the plan as a supplement. It’s one of the reasons that we here at Easy medicare 65 we detail any plan and go over the full summary of benefits and take the puzzle out of the Medicare process for you.
Lawmakers and insurance companies now try to protect people from this by disclaimers on the plan materials. The Medicare Advantage plan Summary of Benefits and Application clearly and repeatedly state that the plan is a Medicare Advantage plan. This aims to protect not only you but also protects insurance agents who often diligently explain that a plan is Medicare Advantage, and yet for some reason the client misses it.
It’s my opinion that this happens because people new to Medicare are inundated with so much information. It’s a lot to absorb. Too many of them get so dazzled by that low premium on the Medicare Advantage plans that they simply fail to listen to the rest of the presentation in which the agent explains how the Advantage plan works.
So the updated Medicare Advantage plan enrollment materials are a first step in preventing this problem.
And now the return of the OEP is a second step in solving this problem. It provides an opt-out period during which beneficiaries who get this wrong, for whatever reason, can change back to Original Medicare or a new MAPD plan.
Since Medicare Advantage plans lock you in for a whole calendar year, thousands of beneficiaries used to get stuck in plans that they didn’t want. Thus now we have the OEP.
Lawmakers realized that by discontinuing the Medicare OEP back in 2010, they forced some Medicare beneficiaries to stay in a plan that they didn’t like for a whole year before they could change. Since beneficiaries often make these mistakes unwittingly, it didn’t seem fair. Therefore, they have reinstated the Medicare Open Enrollment Period, the OEP from January 1st to March 31st. Contact us for more details.
We know this process can be confusing, therefore If you still have any questions, please call us at 407-752-0436 or contact us below. All your information is both private and secure on this site and never used for marketing purposes.
Need more help? Call 407-752-0436 or contact us!
This website is secure!
This secure site uses cookies to analyze website traffic and optimize your website experience. No information is kept or stored for your privacy and security!